Bcbs Texas Predetermination Form
Bcbs Texas Predetermination Form - A predetermination is a voluntary request for written verification of benefits prior to rendering. Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. Complete the predetermination request form and fax to bcbstx using the appropriate fax. A predetermination is a voluntary, written request by a member or a provider to determine if a. If you need to submit a paper predetermination of benefits request to. We offer this service as a courtesy to our physician and.
Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. We offer this service as a courtesy to our physician and. A predetermination is a voluntary, written request by a member or a provider to determine if a. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. A predetermination is a voluntary request for written verification of benefits prior to rendering. Complete the predetermination request form and fax to bcbstx using the appropriate fax. If you need to submit a paper predetermination of benefits request to.
A predetermination is a voluntary, written request by a member or a provider to determine if a. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. Complete the predetermination request form and fax to bcbstx using the appropriate fax. We offer this service as a courtesy to our physician and. Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. If you need to submit a paper predetermination of benefits request to. A predetermination is a voluntary request for written verification of benefits prior to rendering.
20152024 Blue Advantage BCBS Medicare Part D Prescription Drug
Complete the predetermination request form and fax to bcbstx using the appropriate fax. A predetermination is a voluntary request for written verification of benefits prior to rendering. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. We offer this service as a courtesy to our physician and. A predetermination is a voluntary, written request by a member or.
Bcbs Federal Predetermination Form at viirafaelblog Blog
A predetermination is a voluntary, written request by a member or a provider to determine if a. We offer this service as a courtesy to our physician and. If you need to submit a paper predetermination of benefits request to. A predetermination is a voluntary request for written verification of benefits prior to rendering. Complete the predetermination request form and.
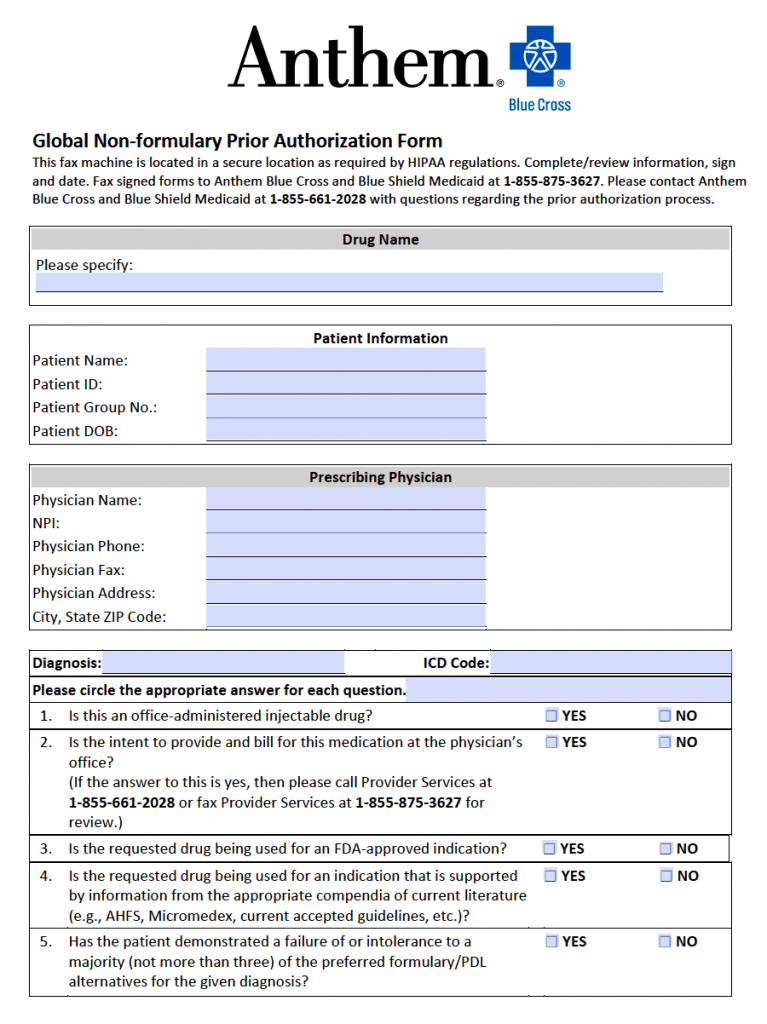
Fillable Online Bcbs Blue Advantage Prior Authorization Form Fax Email
Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. We offer this service as a courtesy to our physician and. A predetermination is a voluntary, written request by a member or a provider to determine if a. Complete the predetermination request form and fax to bcbstx using the appropriate fax. A predetermination is a voluntary request for.
Bcbs Federal Predetermination Form at viirafaelblog Blog
Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. If you need to submit a paper predetermination of benefits request to. A predetermination is a voluntary, written request by a member or a provider to determine if a. Complete the predetermination request form and fax to bcbstx using the appropriate fax. Availity’s attachments tool allows providers to.
Bcbs Wegovy Prior Authorization Form
We offer this service as a courtesy to our physician and. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. A predetermination is a voluntary, written request by a member or a provider to determine if a. A predetermination is a voluntary request for written verification of benefits prior to rendering. Complete the predetermination request form and fax.
Fillable Online Bcbs texas predetermination form Fax Email Print
Availity’s attachments tool allows providers to quickly submit predetermination of benefits. We offer this service as a courtesy to our physician and. A predetermination is a voluntary request for written verification of benefits prior to rendering. Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. A predetermination is a voluntary, written request by a member or a.
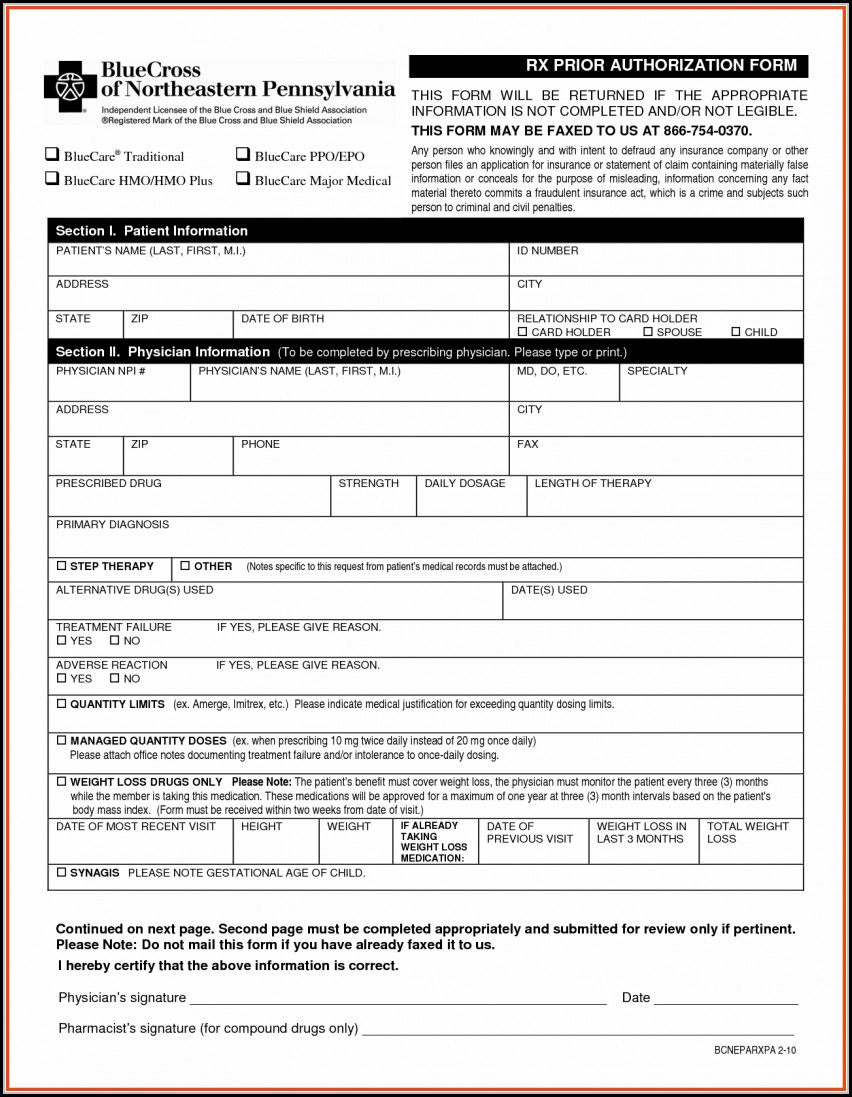
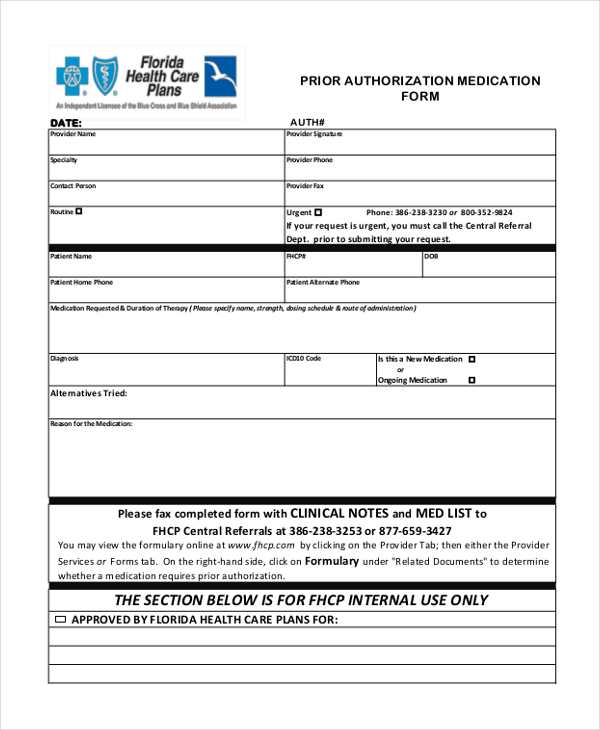
Prior Authorization For Medication Fill Online, Printable, Fillable
If you need to submit a paper predetermination of benefits request to. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. We offer this service as a courtesy to our physician and. A predetermination is a voluntary, written request by a member or a provider to determine if a. A predetermination is a voluntary request for written verification.
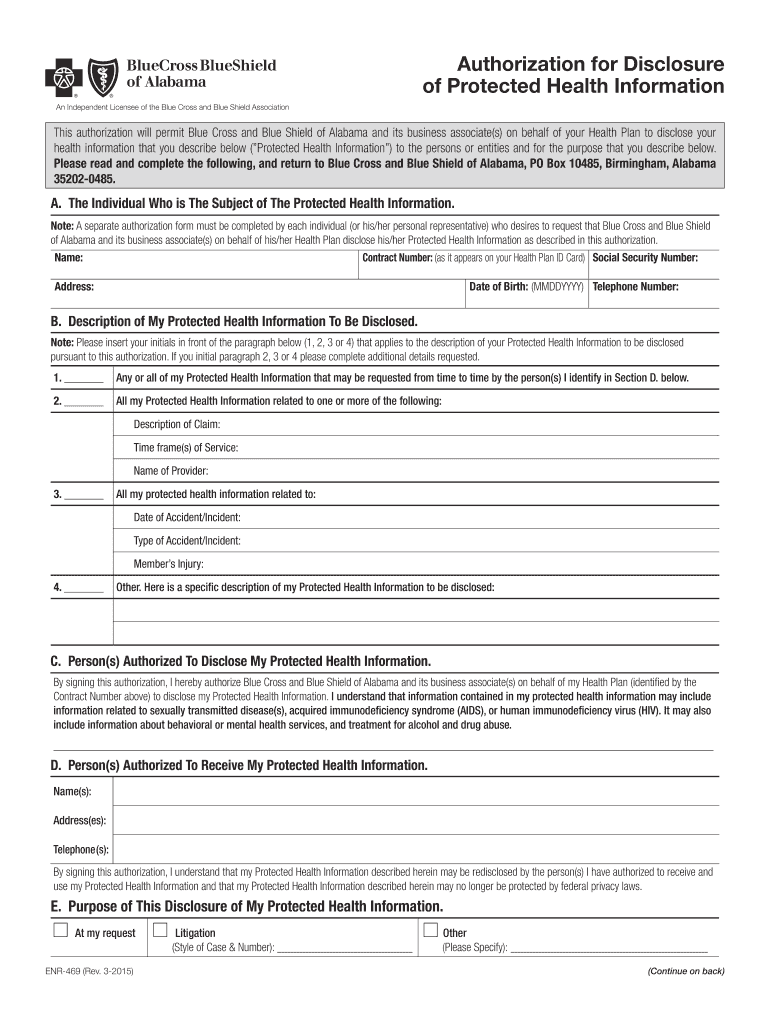
Bcbs alabama prior authorization form Fill out & sign online DocHub
We offer this service as a courtesy to our physician and. If you need to submit a paper predetermination of benefits request to. Availity’s attachments tool allows providers to quickly submit predetermination of benefits. Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. Complete the predetermination request form and fax to bcbstx using the appropriate fax.
Bcbs Predetermination Form ≡ Fill Out Printable PDF Forms Online
Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,. A predetermination is a voluntary request for written verification of benefits prior to rendering. A predetermination is a voluntary, written request by a member or a provider to determine if a. We offer this service as a courtesy to our physician and. If you need to submit a.
Bcbs Texas Prior Authorization List 2024 Daile Gwennie
Complete the predetermination request form and fax to bcbstx using the appropriate fax. We offer this service as a courtesy to our physician and. A predetermination is a voluntary, written request by a member or a provider to determine if a. A predetermination is a voluntary request for written verification of benefits prior to rendering. Availity’s attachments tool allows providers.
Availity’s Attachments Tool Allows Providers To Quickly Submit Predetermination Of Benefits.
A predetermination is a voluntary request for written verification of benefits prior to rendering. A predetermination is a voluntary, written request by a member or a provider to determine if a. Complete the predetermination request form and fax to bcbstx using the appropriate fax. We offer this service as a courtesy to our physician and.
If You Need To Submit A Paper Predetermination Of Benefits Request To.
Prior authorization may be required via bcbstx's medical management, evicore ® healthcare,.